Nursing diagnosis of nephrotic syndrome takes center stage in this comprehensive guide, unraveling the intricacies of this complex condition with an authoritative and engaging approach. Drawing upon a wealth of research and clinical expertise, we delve into the pathophysiology, assessment, management, and patient support strategies, empowering healthcare professionals with the knowledge and tools to deliver optimal care.
Definition and Overview
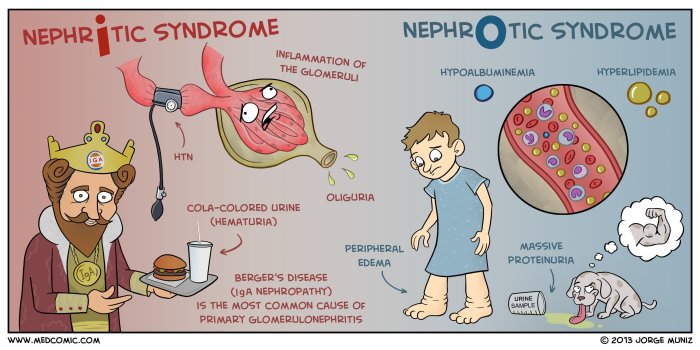
Nephrotic syndrome is a renal disorder characterized by excessive protein loss in the urine, known as proteinuria. It is often caused by glomerular damage, leading to increased permeability and impaired filtration function. Common causes of nephrotic syndrome include glomerulonephritis, diabetic nephropathy, and systemic lupus erythematosus.
Clinical manifestations include edema, especially in the lower extremities and periorbital area, due to fluid retention. Patients may also experience foamy urine, fatigue, and weight gain. The pathophysiology involves impaired glomerular filtration, resulting in proteinuria, hypoalbuminemia, and fluid retention.
Assessment and Diagnosis
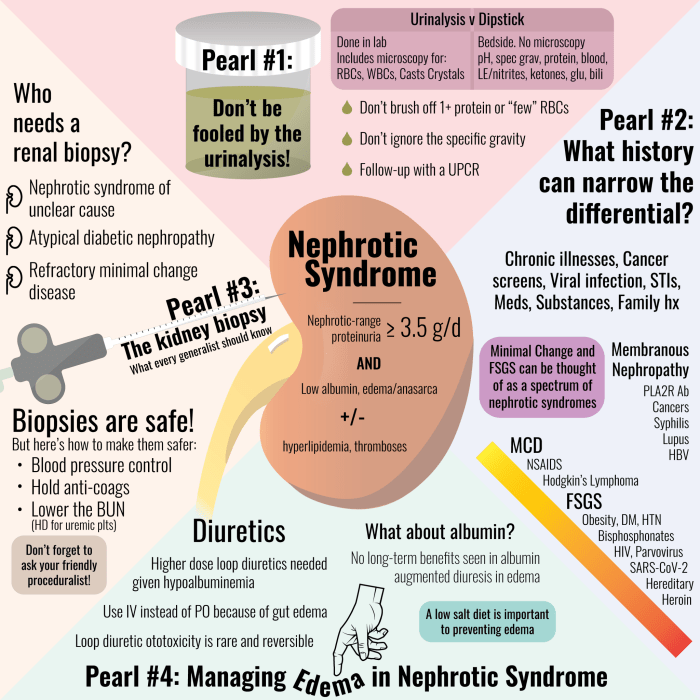
Clinical assessment involves evaluating edema, proteinuria, and other signs and symptoms. Urinalysis reveals proteinuria, while blood tests show hypoalbuminemia, hyperlipidemia, and elevated creatinine levels. A kidney biopsy may be performed to confirm the diagnosis and determine the underlying cause.
Nursing Care Management
Fluid and Electrolyte Management, Nursing diagnosis of nephrotic syndrome
Diuretics are prescribed to promote fluid excretion and reduce edema. Fluid restriction may be necessary to prevent fluid overload. Monitoring electrolytes, especially sodium and potassium, is crucial to maintain balance.
Proteinuria Management
Dietary modifications, such as a low-protein diet, are recommended to reduce protein loss. Medications like angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs) may be prescribed to decrease proteinuria.
Patient Education and Support
Patient education is essential to enhance understanding of the disease, treatment plan, and potential complications. Nurses play a vital role in providing information about medication management, dietary modifications, and lifestyle changes. Support groups and resources can provide emotional and social support to patients and their families.
Interdisciplinary Collaboration
Effective management of nephrotic syndrome requires collaboration among healthcare professionals. Nephrologists provide medical expertise, nurses manage patient care, dietitians guide dietary modifications, and social workers address psychosocial needs. Open communication and coordination ensure continuity of care and optimal patient outcomes.
FAQ Compilation: Nursing Diagnosis Of Nephrotic Syndrome
What are the common symptoms of nephrotic syndrome?
Edema (swelling), proteinuria (protein in urine), hypoalbuminemia (low albumin levels), and hyperlipidemia (high cholesterol and triglycerides).
How is nephrotic syndrome diagnosed?
Through physical examination, urine analysis, blood tests, and kidney biopsy.
What is the role of nurses in managing nephrotic syndrome?
Nurses play a crucial role in assessing symptoms, monitoring fluid and electrolyte balance, administering medications, providing patient education, and collaborating with other healthcare professionals.